What is osteoporosis?
Osteoporosis is a condition that is characterized by bones that are less dense than, and thus not as strong as, normal bone. Osteoporosis increases the risk of breaking bone (fracture) with even minor trauma, such as a fall from standing height, or even from a cough or sneeze. Unfortunately, people often do not realize they have osteoporosis until either they have a fracture or have a screening test ordered by their doctor to check for osteoporosis. Osteoporosis and low bone mass affect an estimated 44 million Americans (National Osteoporosis Foundation 2008). Of those, 10 million have osteoporosis, and the remaining 34 million have a lower than normal bone mass and are at higher risk of developing osteoporosis. Women are four times more likely to develop osteoporosis than men. Other risk factors include older age, family history of osteoporosis, small and thin stature, inactive lifestyle, smoking, alcohol, and use of certain medications including steroids. The treatment and management of osteoporosis is discussed in detail elsewhere on this site. This article will focus on the role of bone mineral density (BMD) evaluation.
How does osteoporosis occur?
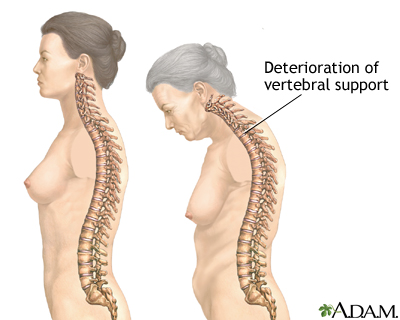
In order to understand the role of bone mineral density scanning, it is important to know a little about how osteoporosis occurs. Bone is constantly being remodeled. This is the natural, healthy state of continuous uptake of old bone (resorption) followed by the deposit of new bone. This turnover is important in keeping bones healthy and in repairing any minor damage that may occur with wear and tear. The cells that lay new bone down are called osteoblasts, and the cells responsible for resorption of old bone are called osteoclasts. Osteoporosis occurs as a result of a mismatch between osteoclast and osteoblast activity. This mismatch can be caused by many different disease states or hormonal changes. It is also commonly a result of aging, change in normal hormones as occurs after menopause, and with diets low in calcium and vitamin D. In osteoporosis, osteoclasts outperform osteoblasts so that more bone is taken up than is laid down. The result is a thinning of the bone with an accompanying loss in bone strength and a greater risk of fracture. A thinning bone results in a lower bone density or bone mass.
There are two major types of bone. Cancellous bone (also known as trabecular bone) is the inner, softer portion of the bone, and cortical bone is the outer, harder layer of bone. Cancellous bone undergoes turnover at a faster rate than cortical bone. As a result, if osteoclast and osteoblast activity become mismatched, cancellous bone is affected more rapidly than cortical bone. Certain areas in the body have a higher ratio of cancellous bone to cortical bone such as the spine (vertebrae), the wrist (distal radius) and the hips (femoral neck).
Most of a person's bone mass is achieved by early adulthood. After that time, the bone mass gradually decline throughout the rest of a person's life. There is a normal rate of decline in bone mass with age in both men and women. For women, in addition to age, the menopause transition itself causes an extra degree of bone loss. This bone loss is greatest in the first three to six years after menopause. Women can lose up to 20% of the total bone mass during this time. Since women generally have a lower bone mass to begin with in comparison with men, the ultimate result is a higher risk of fracture in postmenopausal women as compared to men of the same age. Nevertheless, it is important to remember that men may also be at risk for osteoporosis, especially if they have certain illnesses, a low testosterone level, are smokers, take certain medications, or are sedentary. The best method to prevent osteoporosis is to achieve as high a bone mass by early adulthood with a proper diet and regular exercise. Unfortunately, osteoporosis is not often considered during this time in a person's life.
What is "bone mineral density" (BMD)?
The absolute amount of bone as measured by bone mineral density (BMD) testing generally correlates with bone strength and its ability to bear weight. The BMD is measured with a dual energy x-ray absorptiometry test (referred to as a DEXA scan). By measuring BMD, it is possible to predict fracture risk in the same manner that measuring blood pressure can help predict the risk of stroke.
It is important to remember that BMD cannot predict the certainty of developing a fracture. It can only predict risk. It is also important to note that a bone density scan, or test, should not be confused with a bone scan, which is a nuclear medicine test in which a radioactive tracer is injected that is used to detect tumors, cancer, fractures, and infections in the bone.
The World Health Organization has developed definitions for low bone mass (osteopenia) and osteoporosis. These definitions are based on a T-score. The T-score is a measure of how dense a patient's bone is compared to a normal, healthy 30-year-old adult.
Normal: A bone BMD is considered normal if the T-score is within 1 standard deviation of the normal young adult value. Thus a T-score between 0 and -1 is considered a normal result.
Low bone mass (medically termed osteopenia): A BMD defines osteopenia as a T-score between -1 and -2.5. This signifies an increased fracture risk but does not meet the criteria for osteoporosis.
Osteoporosis: A BMD greater than 2.5 standard deviations from the normal (T score less than or equal to -2.5) defines osteoporosis.
Based on the above criteria, it is estimated that 40% of all postmenopausal Caucasian women have osteopenia and that an additional 7% have osteoporosis.
Why is BMD measurement important?
Determining a person's BMD helps a doctor decide if a person is at increased risk for osteoporosis-related fracture. The purpose of BMD testing is to help predict the risk of future fracture. The information from a BMD is used to aid a decision as to whether prescription medicine therapy is needed to help reduce the risk of fracture. Additionally, if a patient has a fracture or is planning orthopaedic surgery, a diagnosis of osteoporosis might affect the surgical plan. A fracture that could potentially heal in a cast with normal bone mass might require either a longer period of casting or even surgery if the patient has osteoporosis.
What is the relationship between BMD and fracture risk?
In patients with low bone mass at the hip or the spine (the two areas traditionally measured with DEXA scanning), there is a two- to threefold increase in the incidence of any osteoporotic fracture. In other words, low bone density at the measured areas of the spine and hip can even predict future osteoporotic fractures at other parts of the body besides the spine and hip. In subjects with a BMD in the osteoporosis range, there is approximately a five times increase in the occurrence of osteoporotic fractures.

Who should have BMD testing?
BMD testing is recommended for all women over the age of 65. Additionally, postmenopausal women under 65 years who have risk factors for osteoporosis other than menopause (these include a previous history of fractures, low body weight, cigarette smoking, and a family history of fractures) should be tested. Finally, men or women with strong risk factors as listed below should discuss the benefit of DEXA scanning with their doctor to see if testing is indicated.
The following are potential risk factors for osteoporosis that might suggest the need for DEXA scanning:
- personal history of fracture as an adult,
- history of fracture in first-degree relative,
- low body weight or thin body stature,
- advanced age,
- current cigarette smoking,
- use of corticosteroid therapy for more than three months,
- impaired vision,
- estrogen deficiency at early age,
- dementia,
- poor health/frailty,
- recent falls,
- lifelong low calcium intake,
- low physical activity,
- alcohol intake of more than two drinks/day,
- thyroid disease,
- rheumatoid arthritis,
- excessive caffeine consumption, and
- use of oral contraceptive (birth control pills).
How is BMD measured?
Dual energy X-ray absorptiometry, or DEXA, is the most common method to measure a patient's BMD. DEXA is relatively easy to perform and the amount of radiation exposure is low. A DEXA scanner is a machine that produces two X-ray beams, each with different energy levels. One beam is high energy while the other is low energy. The amount of X-rays that pass through the bone is measured for each beam. This will vary depending on the thickness of the bone. Based on the difference between the two beams, the bone density can be measured. The radiation exposure from a DEXA scan is actually much less than that from a traditional chest X-ray.
At present, DEXA scanning focuses on two main areas, the hip and spine. Although osteoporosis involves the whole body, measurements of BMD at one site can be predictive of fractures at other sites. Scanning generally takes 10 to 20 minutes to complete and is painless. The patient needs to be able to lay still on the table during the testing. There is no IV or other injection needed for this test. On the day of the test, you may eat a normal meal, but you should not take any calcium supplements for 24 hours prior to the test.
Certain conditions can alter the results of the DEXA scan, making result less reliable. These include a lumbar spinal deformity (scoliosis), a large amount of calcium in the blood vessels (atherosclerosis), or multiple fractures. These conditions can falsely elevate the measured BMD with the DEXA scan.
What are other methods of measuring BMD?
There are small DEXA scanners called peripheral DEXA machines. These machines often measure BMD at the heel (calcaneus), shin bone (distal tibia), or kneecap (patella). Regular DEXA machines have a standard reference (called NHANES III) that can be used for all machines, no matter the manufacturer. However, peripheral DEXA machines do not yet have a uniform reference standard for the normal peak young adult bone mass that can apply to all machines and all manufacturers. This is necessary for peripheral DEXA to be ready for more widespread use. Efforts are in progress to make the peripheral DEXA technique more standardized.

Quantitative computed tomography (QCT) can be used to assess BMD. A standard CT scanner is used in this method. However, the amount of radiation exposure is higher than with DEXA and the cost is greater. For these reasons, QCT is not in general clinical use.
Ultrasound is a relatively new diagnostic tool to measure BMD. There is no radiation source with this procedure. An ultrasound beam is directed at the area being analyzed. The scattering and absorption of the waves allow for an assessment of bone density. The results are not as precise as with the other methods mentioned. This technique is relatively new, and there is considerable research being conducted in this area. Since ultrasounds can easily be performed in a physician's office, this method may become valuable for screening larger populations if its accuracy becomes more refined. If the BMD is low on the ultrasound test, you might be asked to have a DEXA scan to confirm the results.
How often should DEXA scans be repeated to monitor treatment?
Monitoring osteoporosis treatment using DEXA scans is highly controversial. Some doctors recommend DEXA scanning at one- to two-year intervals to monitor changes in bone density during treatment. But recent scientific evidence questions the usefulness of such interval monitoring. Reasons why repeating bone density scans is extremely tricky include:
- Bone density changes so slowly that the changes may be smaller than the measurement error of the machine. In other words, repeat DEXA scans cannot distinguish between a "real" increase in bone density or a mere variation in measurement from the machine itself. Typically, BMD changes 1% per year, which is less than the error of a DEXA machine (usually in the range of 3%). Changes of less than 2%-4% in the vertebrae and 3%-6% at the hip from test to test can be due to the precision error of the method.
- Whereas the real purpose of prescription osteoporosis treatment is to decrease future bone fractures, there is no good correlation between increases in bone density as measured by DEXA with decreases in fracture risks with treatment. There are multiple examples of this in recent clinical studies. For example, the improvement in BMD only accounted for 4% of the reduction in spine fracture risk with raloxifene, 16% of the reduction in spine fracture risk with alendronate, and 18% of the reduction in spine fracture risk with risedronate. Thus, improvement in BMD does not indicate the amount of the anti-fracture benefit of osteoporosis medication. Prescription medication may decrease a person's risk of fracture even when there is no apparent increase in BMD. Physicians and non-physicians alike are often surprised to learn this information.
- Even if the DEXA scan shows continued deterioration in bone density during treatment, no research data exists demonstrating that changing a medication, combining medications, or increasing medication doses will be safe and helpful in decreasing the future risk of fractures compared to just continuing the same medication.
- Even if a person's bone density deteriorates during treatment, it is quite likely that the person would have lost even more bone density without treatment.
- Recent research has shown that women who lose bone density after the first year of menopausal hormone therapy will gain bone density in the next two years, whereas women who gain in the first year will tend to lose density in the next two years of therapy. Therefore, bone density during treatment naturally fluctuates and may not be indicative of the fracture protection of the medication.
What is the cost of DEXA?
The cost for DEXA scanning varies depending on insurance policies and coverage. In general, a patient without coverage paying cash can expect to pay approximately $200 U.S. for the procedure.
What about the accuracy of BMD testing in the doctor's office using smaller equipment?
There are several devices that are smaller than the standard DEXA scanners that are being used in doctors offices to screen for low bone density. Very little scientific data is available about these smaller units. Most of the information comes directly from the equipment manufacturers themselves. Many of these models test peripheral bones in the feet or hands. Other units use ultrasonography. These techniques can be less accurate than BMD testing performed with state of the art equipment. Additionally, office-testing equipment can range dramatically in price and quality.
In general, these devices may be reasonable to measure overall fracture risk but are not useful in monitoring therapy. Their use might be limited to screening and results would require confirmation using DEXA. In addition, expertise in using the equipment and interpreting the data can vary. At present, it is difficult to comment on these other methods of BMD testing. Some doctors use these as screening tools and recommend more formal DEXA testing if they are abnormal.
Summary
Osteoporosis is a disease that results in a significant risk of fracture. The consequences of fracture can include hospitalization, immobility, a decrease in the quality of life, and even death. From a larger perspective, it is a costly disease in terms of the health-care system and time lost from work. Early detection and therapy is the mainstay for trying to prevent these complications. BMD testing results correlate well with the risk of fracture, and the testing is easily performed in a time-efficient manner without any discomfort. Although many methods of BMD testing exist, the best currently is DEXA scanning. It is imperative that testing ultimately be done using state-of-the-art equipment with capable highly-trained personnel and a doctor well versed in interpreting the results.
Bone Density Scan At A Glance
- 40% of postmenopausal women in the U.S. have osteopenia (low bone density). An additional 7% have osteoporosis.
- In 1995, osteoporosis-related fractures were associated with over 400,000 hospitalizations, stressing the importance of early detection and appropriate prescription therapy.
- Bone mineral density (BMD) estimates the true mass of bone.
- BMD analysis is recommended for women between ages 50 and 65 with risk factors for osteoporosis and for all women over the age of 65. In addition, men and women taking certain medications or having certain diseases should discuss testing with their doctor.
- By measuring BMD, it is possible to predict fracture risk in the same manner that measuring blood pressure can help predict the risk of stroke.
- DEXA is quick, painless and the preferred method to measure BMD.
- Osteoporosis has many available prescription and nonprescription treatment options once the diagnosis is made.
Previous contributing author: Medical Revising Author: Carolyn J. Crandall, MD, FACP
References:
Cummings, et al. Am J Med 2002.
Gelbach, et al. Osteoporosis International 2003.
Marshall, et al. BMJ 1996.
National Osteoporosis Foundation Physician's Guide to Prevention and Treatment of Osteoporosis 2003.
Sarkar, et al. JBMR 2001.
Siris, et al. JAMA 2001.
Watts, et al. J Clin Densitom 2004.
Last Editorial Review: 4/11/2008
|
Bookmark this post:
|
|

0 comments
Post a Comment