First of all, here she is right now admiring her mother. This little girl has been through a LOT in the last couple days. Lots of emotions, and this place is swirling with miracles.
Ok now here is some of the back story getting to this point. Tuesday night (the night before the second cath procedure) was crazy. Finding that balance between allowing the ductus to close just enough for the stent without totally closing and without staying too big can be pretty tricky! Especially when you have a feisty baby girl who wants to eat but can’t! If the oxygen saturation in her blood drops too low it is a clear indication that the hole is closing. SO the goal for Tuesday night was to be in the 75-85% range up until close to 7AM (and ideally the levels dropping around that time indicating that the ductus is closing and ready for the stent). Then at 7AM - another echocardiogram to make sure the ductus is a good size before going into the cath lab.
We watched the numbers on the screen somewhat anxiously for several hours and things seemed pretty good (there was an occasional drop but always a rebound). At around 9:15, we ran outside to get something to eat (no food allowed in the CTICU) and when we got back at around 10, Dr. Ing (the one performing the catheter procedure) and other doctors were with Shelby because her O2 saturation had dropped hitting into the mid to high 60s and they were worried the ductus was closing. They started the PGE again and put some oxygen in her nose and she responded immediately and the levels came up to the low 80s again. Figuring the rapid rise was from the oxygen and not the PGE, they turned the PGE back off and the levels were right on so it seemed that the ductus was still quite open. Dr. Ing instructed the nurses to use a little more oxygen if needed and that if the levels drop even with increased oxygen to call his cell phone and he’d decide how to proceed. We felt much more comfortable knowing the oxygen in the nose was keeping things stable and that Dr. Ing was just a phone call away.
The red light on her toe in this picture is what measures the oxygen saturation levels.

From about 1am until 3am Shelby was HUNGRY. She was going crazy and the nurses and Kristi and I were taking turns trying to sooth her. We learned that it can get pretty tricky soothing a baby who is hooked up to all kinds of wires while worrying about oxygen levels! Particularly when you have the solution right there in your boobs but you can’t give it! We even tried this awesome high tech swing thing - which worked for about 3 minutes. The nurses were phenomenal – talking so sweetly to the baby and being so patient. Her O2 stats were fluctuating and making us anxious but luckily they always returned to the right levels.
At one point there was a nurse from next door helping while our nurse was on a break and he insisted that we go to bed to try to get some sleep and took her. As he calmed her down we could hear him through the curtain quietly singing to her. It was pretty sweet and made us feel so grateful for these awesome people that dedicate their life profession to helping others.
We figured we could both sleep here on this tiny bed if we put our heads on opposite ends and it worked pretty well but around 4am this feisty little girl got MAD again and even managed to kick one of her IV lines out of her umbilical vein so the nurses had to put another IV into the tiny veins in her hand!
Through all of this, even with the anxiety and worry and sleep deprivation, we felt this underlying peace and assurance that our prayers were being answered.
Here they are putting the IV into her hand.

New IV in and ready to go.

At 7am the saturation started to drop once again- this time according to plan. Perfect! They came in and did an echocardiogram and sure enough the ductus was right where it needed to be between 2.5mm and 3.5mm (Dr. Ing was looking for 3mm). Relief. Again a wave of peace came over us with a deep assurance that this was a clear answer to the tremendous amount of faith and prayers being said by so many.
Here they are checking the size of the ductus.

After the ultrasound they whisked her down the hall to the cath lab and we left our baby in the Doctors’ very capable hands.


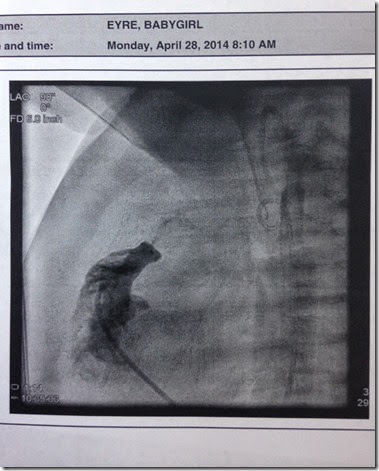
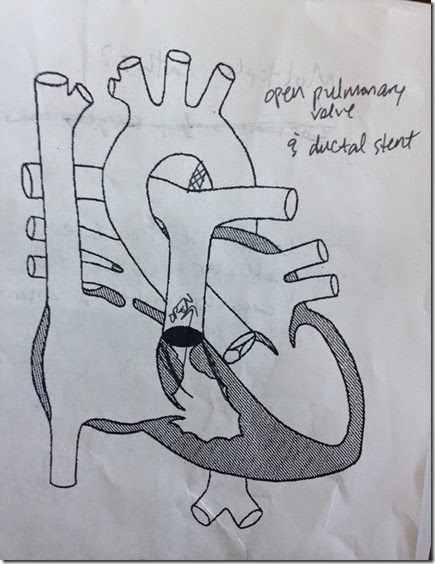
After a little breakfast and a couple hours of slightly impatient waiting, they called the nurse to tell us to come to the consult room for the results. So we headed over. And waited. And waited. We sat there long enough to worry about what they would say and then Dr. Ing came in smiling and just started talking about the stent in there like it was no big deal and we were like “it’s in?!” and he’s like “yeah, it’s in, actually two of them.” (the ductus was longer than normal so they put two for additional length)! He said things went really well and that by the time they got in the ductus was about 1.8mm in diameter on one side and about 4mm on the other which was fine because he was able to get a 3.8mm stent pushed through there and secured on one side and felt confident that it will hold strong while the rest closed down around it. We got to talk for a while about next steps and asked a lot of questions but the whole time flowing inside us through the conversation was a deep sense of gratitude. As Shelby’s little 5 year old cousin Braden put it “our prayers were answered!”
Dr. Ing explained that as long as things go well with the right heart flow and that the muscle in the ductus grows tight around the stents, we may be able to take her home in the next week or so!!!! Going into this, we were expecting her to have a minimum of 3 open heart surgeries – and there are likely to still be surgeries down the road but it is a TOTAL MIRACLE that they were able to do everything by cath through the veins and arteries! Blows us away every time we think of it! Opening a valve and putting stents in through the veins?! Seriously!?
When we got back to the room she was still out from the anesthesia. And continued to be out for a long time. She started to react to touch some but she was not breathing very well – relying on a ventilator to keep her breathing. She would take breaths when we would touch her but then she would get all comfy and relax and just “ride the machine” as they call it. So they had to secure the tube in her mouth for the next several hours. They continued to try to wean her off of the ventilator and she would breathe for a while but kept having spouts of apnea and kept riding the ventilator. Finally by early morning today she woke up and was uncomfortable with the tube down her throat among other things so she was upset – totally awake, breathing, and crying (one of the few times where a mad baby is a huge blessing). And this is the part that breaks your heart a little - that breathing tube goes through the vocal cords and it is not comfortable so she was clearly making a waling cry but it was totally silent. It was an interesting mix of emotion to see her alert and awake and breathing and crying but silent.

I know we may be bias but we think she is pretty cute even when all taped up

She got more and more consistent with taking her own breaths through the morning and they were able to take the breathing tube out by about 11:30! Little by little, she will shed all the cords and IVs and wires connected to her over the next few days.
And we will finish this update with this picture – her first feed!! We have been saving Kristi’s milk and just now for the first time, Shelby ate! First through a bottle but nursing is just around the corner! And viola! - boob solution!