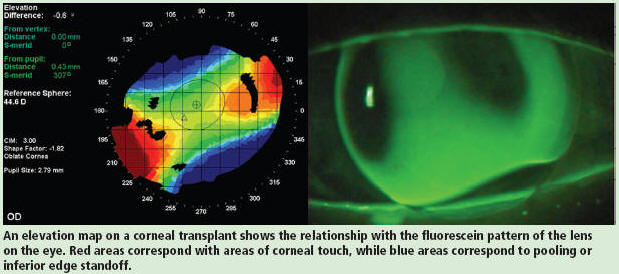
The rapid growth in laser and photonic technology has resulted in new tools being proposed and developed for use in the medical and biological sciences. Specifically, a discipline known as biomedical optics has emerged which is providing a broad variety of optical techniques and instruments for diagnostic, therapeutic and basic science applications. New laser sources, detectors and measurement techniques are yielding powerful new methods for the study of diseases on all scales, from single molecules, to specific tissues and whole organs. For example, novel laser microscopes permit spectroscopic and force measurements to be performed on single protein molecules; new optical devices provide information on molecular dynamics and structure to perform `optical biopsy’ non-invasively and almost instantaneously; and optical coherence tomography and diffuse optical tomography allow visualization of specific tissues and organs. Using genetic promoters to derive luciferase expression, bioluminescence methods can generate molecular light switches, which serve as functional indicator lights reporting cellular conditions and responses in living animals. This technique could allow rapid assessment of and response to the effects of anti-tumour drugs, antibiotics, or antiviral drugs.
This issue of Physics in Medicine and Biology highlights recent research in biomedical optics, and is based on invited contributions to the International Conference on Advanced Laser Technology (Focused on Biomedical Optics) held at Cranfield University at Silsoe on 19–23 September 2003. This meeting included sessions devoted to: diffuse optical imaging and spectroscopy; optical coherence tomography and coherent domain techniques; optical sensing and applications in life science; microscopic, spectroscopic and opto-acoustic imaging; therapeutic and diagnostic applications; and laser interaction with organic and inorganic materials.
Twenty-one papers are included in this special issue. The first paper gives an overview on the current status of scanning laser ophthalmoscopy and its role in bioscience and medicine, while the second paper describes the current problems in tissue engineering and the potential role for optical coherence tomography. The following seven papers present and discuss latest developments in infrared spectroscopy and diffuse optical tomography for medical diagnostics. Eight further papers report recent advances in optical coherence tomography, covering new and evolving methods and instrumentation, theoretical and numerical modelling, and its clinical applications. The remaining papers cover miscellaneous topics in biomedical optics, including new developments in opto-acoustic imaging techniques, laser speckle imaging of blood flow in microcirculations, and potential of hollow-core photonic-crystal fibres for laser dentistry.